Abstract
Background: A restrictive transfusion strategy has been shown to be equivalent to a liberal transfusion strategy in terms of mortality and morbidity outcomes in major clinical trials.Liberal transfusions have been associated with higher mortality and morbidity, as well as longer lengths of stay in hospital based on observational data. Although patient blood management programs have reduced transfusion rates and improved patient outcomes, these programs have not been universally applied. Recent province wide audits of frozen plasma (FP) use in Ontario showed a high rate of inappropriate transfusions. Similarly, a recent red blood cell (RBC) audit in Ontario showed that approximately 25% of RBC units transfused were inappropriate.
Objectives: The primary aim of this study was to compare transfusion rates of RBCs and FP across 60 Ontario community hospitals with more than 50 active treatment beds from 2012-2016. The secondary aims were to identify clinical and hospital factors, which may account for these differences.
Methods:This study was a retrospective review of transfusion data from Ontario community hospitals between 2012-2016. RBC and FP transfusion data were acquired through the Canadian Blood Services data warehouse. Acute inpatient bed days and the annual average number of active treatment beds were obtained through the Ministry of Health and Long Term Care of Ontario. Annual transfusion rates were reported as FP and RBC units transfused per 100 acute inpatient days (AIPD), using descriptive statistics. Rates of blood component use were correlated with size of hospital using linear regression to determine whether size of hospital impacted on transfusion practices. Rates of RBC transfusion were correlated with rates of FP transfusion using linear regression. Finally, available data on local transfusion guidelines and pre-existing quality improvement mechanisms, such as pre-printed order sets, the presence of transfusion guidelines at each site were surveyed and reviewed to determine the impact of institutional culture on transfusion practices.
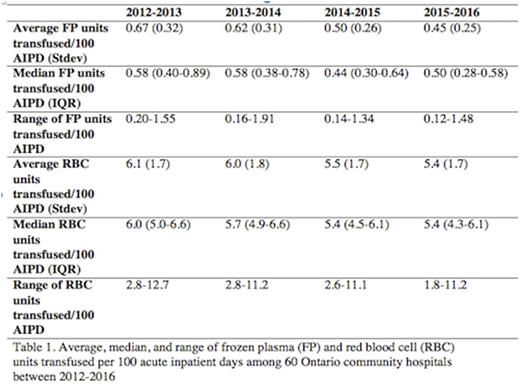
Results: From 2012 to 2016, there were decreasing rates of RBC and FP use over time, with a wide range of variation amongst hospitals (Table 1). The average number of FP units transfused was 0.67, 0.62, 0.50, and 0.44 units per 100 AIPD for 2012-2013, 2013-2014, 2014-2015, and 2015-2016 respectively.The average number of RBC units transfused was 6.1, 6.0, 5.5, and 5.4 units per 100 AIPD for 2012-2013, 2013-2014, 2014-2015, and 2015-2016 respectively. Larger hospitals were associated with a significantly higher FP transfusion rate (p<0.05 for all years). However, there was no correlation between RBC transfusion rates and size of hospital. Of the 24 hospitals that responded to the survey, sites with transfusion quality improvement indicators (N=19) had statistically fewer units of FP transfused (p=0.04 for 2014-2015, p<0.01 for 2015-2016), and had a decrease in the units of FPs transfused from year to year. There was a statistically significant association between FP transfusion rates and RBC transfusion rates (p<0.01 for all years).
Conclusion and significance: There may be cultural differences at different institutions contributing to the variations in transfusion rates across Ontario community hospitals. Characterization of transfusion practices and understanding of institutional culture surrounding blood component use will hopefully lead to quality improvement (QI) initiatives aimed at creating better guidelines, education, and transfusion order entry systems. These data will serve as a baseline to highlight sites and practices where QI initiatives may be most beneficial and potentially replicated in other provinces and states.
Lin: Pfizer: Other: advisory board; Pfizer: Honoraria; Novartis: Research Funding; CSL Behring, Grifols: Other: unrestricted education grant.
Author notes
Asterisk with author names denotes non-ASH members.